Omega-3 fatty acids, especially EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid), have become a cornerstone of discussions around heart health. While these essential fats are naturally found in fatty fish and some plant sources, omega-3 supplements—primarily fish oil—are widely used to support cardiovascular wellness. This article provides an in-depth, research-backed exploration of how omega-3 supplements affect heart health, the mechanisms involved, the evidence from major clinical trials, and practical recommendations for their use.
Contents
- What Are Omega-3 Fatty Acids?
- How Omega-3s Benefit the Heart
- Mechanisms by Which Omega-3s Affect Heart Health
- Evidence from Major Clinical Trials
- Early Trials: Promising Results
- Recent Large-Scale Trials: Mixed Outcomes
- Summary of Major Omega-3 Clinical Trials
- Meta-Analyses and Systematic Reviews
- Effects of Omega-3 Supplementation (Meta-Analysis Data)
- Why Do Studies Show Different Results?
- Recommendations from Leading Health Organizations
- American Heart Association (AHA)
- Recommended Dietary Sources of Omega-3s
- Omega-3 Index: A Personalized Approach
- Safety and Side Effects
- Practical Considerations
- Frequently Asked Questions
- Conclusion
- References
What Are Omega-3 Fatty Acids?
Omega-3s are a family of polyunsaturated fats crucial for human health. The three main types are:
- ALA (alpha-linolenic acid): Found in plant oils like flaxseed, canola, and walnuts.
- EPA (eicosapentaenoic acid): Found in marine sources such as fatty fish.
- DHA (docosahexaenoic acid): Also found in fatty fish and algae.
While ALA is essential and must be obtained from the diet, EPA and DHA are considered the most beneficial for heart health.
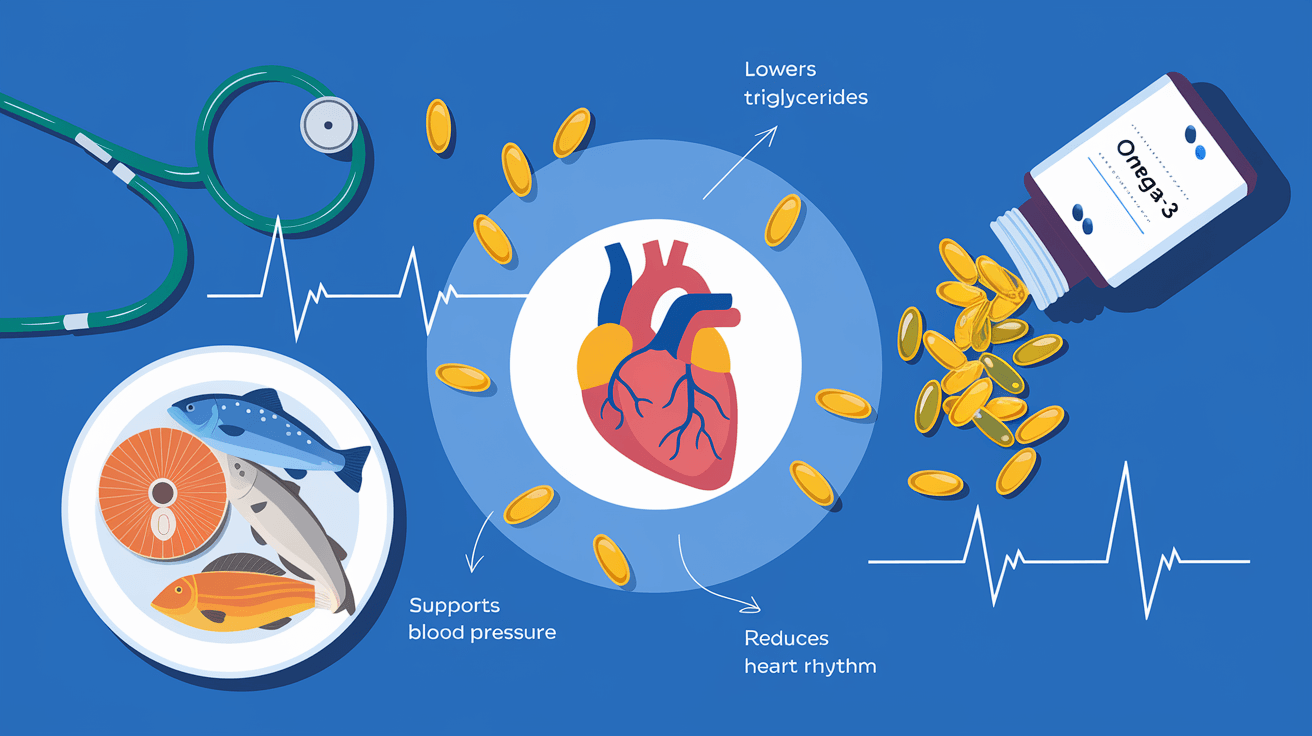
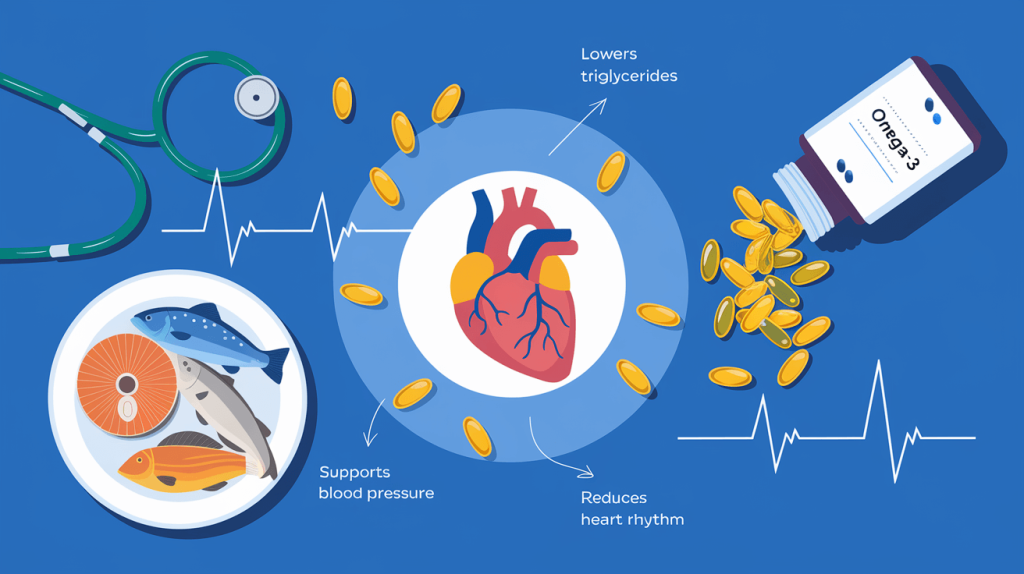
How Omega-3s Benefit the Heart
Omega-3s support cardiovascular health through several mechanisms:
- Lowering Triglycerides: Omega-3s reduce triglyceride levels, which are a risk factor for heart disease.
- Reducing Arrhythmias: They help stabilize heart rhythms and reduce the risk of abnormal heartbeats.
- Slowing Plaque Buildup: Omega-3s slow the development of plaque in arteries, reducing the risk of atherosclerosis.
- Lowering Blood Pressure: Regular intake can help reduce both systolic and diastolic blood pressure.
- Anti-Inflammatory Effects: They decrease inflammation, which plays a role in heart disease progression.
- Improving Endothelial Function: Omega-3s enhance the health of blood vessel linings, supporting better circulation.
Mechanisms by Which Omega-3s Affect Heart Health
| Mechanism | Effect on Heart Health |
|---|---|
| Lower triglycerides | Reduces risk of coronary artery disease |
| Reduce arrhythmias | Lowers risk of sudden cardiac death |
| Slow plaque buildup | Prevents artery blockage |
| Lower blood pressure | Reduces hypertension risk |
| Anti-inflammatory effects | Slows atherosclerosis progression |
| Improve endothelial function | Enhances vessel flexibility |
Evidence from Major Clinical Trials
Early Trials: Promising Results
Early studies and meta-analyses indicated significant cardiovascular benefits for those who consumed omega-3-rich diets or supplements. For example, individuals eating fatty fish several times a week had nearly half the risk of death from coronary heart disease compared to those who did not consume fish. Supplementation was also associated with a 15% reduction in death, heart attack, and stroke incidence, and a 45% reduction in sudden cardiac death in some large trials.
Recent Large-Scale Trials: Mixed Outcomes
However, more recent randomized controlled trials (RCTs) have produced mixed results, especially in primary prevention (preventing heart disease in healthy people).
- VITAL Trial: Over 25,000 healthy participants took 840 mg/day of EPA+DHA or placebo for five years. The trial found no significant reduction in major cardiovascular events overall, but did note a 28% reduction in heart attacks and greater benefits for individuals with low fish intake or of African American descent.
- STRENGTH Trial: Involving 13,078 high-risk participants, this study used 4 g/day of omega-3s and found no significant difference in cardiovascular events compared to placebo.
- REDUCE-IT Trial: Focused on high-risk patients with elevated triglycerides, this trial used 4 g/day of pure EPA and found a 25% reduction in major adverse cardiac events.
Summary of Major Omega-3 Clinical Trials
| Trial Name | Population | Dose & Type | Main Findings |
|---|---|---|---|
| VITAL | Healthy adults | 840 mg EPA+DHA | No overall CVD benefit; ↓ MI in subgroups |
| STRENGTH | High CVD risk | 4 g EPA+DHA | No significant benefit |
| REDUCE-IT | High triglycerides | 4 g EPA | 25% ↓ in major cardiac events |
| GISSI-HF | Heart failure | 1 g EPA+DHA | ↓ CV mortality and hospitalizations |
Meta-Analyses and Systematic Reviews
Meta-analyses pooling data from multiple trials provide a broader perspective:
- Triglyceride and LDL Reduction: Omega-3 supplementation lowers triglycerides by an average of 4.4 mg/dL and modestly decreases LDL cholesterol.
- Major Cardiovascular Events: Omega-3s are associated with a 10% reduction in the risk of major cardiovascular events and a 35% reduction in cardiac mortality.
- Blood Pressure: The optimal intake for blood pressure reduction is between 2–3 g/day, with greater benefits in hypertensive and hyperlipidemic populations.
Effects of Omega-3 Supplementation (Meta-Analysis Data)
| Outcome | Effect Size |
|---|---|
| Triglyceride reduction | -4.4 mg/dL |
| LDL cholesterol reduction | -0.7 mg/dL |
| Major cardiovascular events | 10% risk reduction |
| Cardiac mortality | 35% risk reduction |
| Systolic BP (2–3 g/day) | ↓ 2–4.5 mmHg |
Why Do Studies Show Different Results?
Several factors explain the variability in trial outcomes:
- Dosage: Higher doses (e.g., 4 g/day) show more pronounced benefits, especially in high-risk groups.
- Population: Benefits are clearer in those with existing heart disease, high triglycerides, or certain risk factors.
- Type of Omega-3: EPA-only supplements (like in REDUCE-IT) may be more effective than mixed EPA/DHA products.
- Background Therapy: Modern cardiovascular treatments (statins, antihypertensives) may mask the incremental benefit of omega-3s.
- Placebo Choice: Some trials used corn oil, which may have confounding effects.
Recommendations from Leading Health Organizations
American Heart Association (AHA)
- General Population: Eat at least two servings of fatty fish per week.
- Secondary Prevention: Consider 1 g/day EPA+DHA for those with a history of heart attack or heart failure.
- Hypertriglyceridemia: Prescription omega-3s (2–4 g/day) are recommended for those with very high triglycerides.
Recommended Dietary Sources of Omega-3s
| Food Source | EPA+DHA Content (g/3 oz) | Servings Needed for 1 g EPA+DHA |
|---|---|---|
| Salmon (Atlantic, farmed) | 1.09–1.83 | 1.5–2.5 |
| Sardines | 0.98–1.70 | 2–3 |
| Mackerel | 0.34–1.57 | 2–8.5 |
| Herring (Atlantic) | 1.71 | 2 |
| Tuna (white, canned) | 0.73 | 4 |
| Cod liver oil | 0.19 (per capsule) | 5 |
| Standard fish oil | 0.30 (per capsule) | 3 |
Omega-3 Index: A Personalized Approach
The omega-3 index measures the percentage of EPA and DHA in red blood cells and is emerging as a predictive biomarker for cardiovascular risk:
- <4%: High risk for heart disease
- 4–8%: Intermediate risk
- ≥8%: Optimal protection
Testing your omega-3 index can help tailor supplementation to individual needs.
Safety and Side Effects
Omega-3 supplements are generally safe at doses up to 3 grams per day. Possible side effects include:
- Mild gastrointestinal discomfort
- Fishy aftertaste
- Increased bleeding risk at high doses (>3 g/day)
People on blood thinners or with bleeding disorders should consult their doctor before starting supplementation.
Practical Considerations
- Who Benefits Most?
- People with high triglycerides
- Patients with existing heart disease or heart failure
- Those with low dietary intake of omega-3s
- Certain ethnic groups (e.g., African Americans) may see greater benefit
- How to Choose a Supplement
- Look for products providing at least 500–1000 mg of combined EPA and DHA per serving.
- Prescription omega-3s are recommended for those with very high triglycerides.
- Diet vs. Supplements
- Whole food sources are preferred for most people.
- Supplements are useful for those who do not eat fish or need higher doses for medical reasons.
Frequently Asked Questions
Q: Can omega-3 supplements replace heart medications?
A: No. Omega-3s can support heart health but should not replace prescribed medications for blood pressure, cholesterol, or heart disease.
Q: Are plant-based omega-3s (ALA) as effective as fish-based (EPA/DHA)?
A: ALA has benefits, but EPA and DHA have the strongest evidence for heart health. The body converts ALA to EPA and DHA inefficiently.
Q: How long does it take to see benefits?
A: Improvements in triglycerides and inflammation can be seen within weeks to months, but cardiovascular event reduction is a long-term benefit.
Conclusion
Omega-3 supplements, especially at higher doses and in high-risk populations, offer measurable benefits for heart health, including lowering triglycerides, reducing major cardiovascular events, and decreasing cardiac mortality. While the evidence is mixed for primary prevention in healthy individuals, those with heart disease, high triglycerides, or low dietary intake stand to benefit most. The best approach is to prioritize dietary sources of omega-3s and use supplements as needed, guided by individual risk factors and in consultation with a healthcare provider.
References
- Dempsey M, et al.
“The influence of dietary and supplemental omega-3 fatty acids on cardiovascular disease risk”
Nutrients. 2023.
https://doi.org/10.3390/nu15030638 - Logan SL, et al.
“Omega-3 Fatty Acid Supplementation for 12 Weeks Improves Metabolic Rate in Older Females”
PLOS ONE. 2015.
https://doi.org/10.1371/journal.pone.0144828 - Huang L, et al.
“Effect of Omega-3 Polyunsaturated Fatty Acids on Cardiovascular Outcomes in Diabetic Patients”
American Heart Journal. 2023.
https://doi.org/10.1016/j.ahj.2023.05.004 - Gencer B, et al.
“Marine Omega-3 Fatty Acids and Atrial Fibrillation Risk: A Meta-Analysis of Randomized Trials”
Circulation. 2021.
https://doi.org/10.1161/CIRCULATIONAHA.121.055654 - Yan J, et al.
“Efficacy and Safety of Omega-3 Fatty Acids in Cardiovascular Disease Prevention”
Cardiovascular Drugs and Therapy. 2024.
https://doi.org/10.1007/s10557-022-07362-8 - Hooper L, et al.
“Omega-3 Supplements for Cardiovascular Health: A Cochrane Systematic Review”
Cochrane Database of Systematic Reviews. 2018.
https://www.medicalnewstoday.com/articles/322512 - Vinot N, et al.
“Omega-3 Fatty Acids from Fish Oil Lower Anxiety and Improve Cognitive Function in Primates”
PLOS ONE. 2011.
https://doi.org/10.1371/journal.pone.0020491 - Alfaddagh A, et al.
“Omega-3 Fatty Acids and Reduction of Cardiovascular Inflammation”
Journal of the American Heart Association. 2020.
https://doi.org/10.1161/JAHA.119.014963 - Bhatt DL, et al.
“Cardiovascular Risk Reduction with Icosapent Ethyl: Results from the REDUCE-IT Trial”
New England Journal of Medicine. 2019.
https://doi.org/10.1056/NEJMoa1812792 - Harris WS, et al.
“Omega-3 Index as a Biomarker for Cardiovascular Risk Stratification”
American Journal of Clinical Nutrition. 2021.
https://doi.org/10.1093/ajcn/nqab195
Dr. Emily Carter, MD
Dr. Emily Carter is a board-certified physician specializing in nutrition and preventive medicine. With over 12 years of experience in clinical practice, Dr. Carter is committed to helping people achieve optimal health through evidence-based dietary choices and lifestyle interventions. She earned her medical degree from King’s College London and completed her residency at St. Mary’s Hospital.
Dr. Carter has contributed to numerous medical journals and is recognized for her ability to translate complex scientific research into clear, actionable guidance for the public. She is passionate about patient education and believes in empowering individuals to make informed decisions about their health and wellness.
Outside of her medical work, Dr. Carter enjoys gardening, reading historical novels, and participating in local health outreach programs.